In a world where organ transplants are scarce, printing organs using biotechnology is a lifeline. Biomedical engineering and regenerative medicine are turning theoretical possibilities into clinical reality. Bioprinting living tissues and organs is a futuristic and increasingly practical solution to organ shortages, chronic diseases, and catastrophic injuries. It’s happening in labs around the world, not science fiction.
Bioprinting involves creating complex biological structures that function like the human body, rather than just covering it with cells. Scientists are printing life using powerful printers, bioinks made from living cells, and sophisticated computer models. The applications are broad and growing, from skin grafts for burn victims to drug testing on liver tissue. At this rate, bioprinted hearts, kidneys, and lungs could be used in transplants, revolutionizing our understanding of human health and longevity.
Learn About the Science Behind Organ Bioprinting
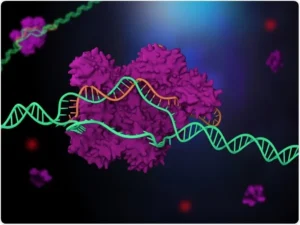
Organ bioprinting is an additive manufacturing technique that uses bioinks (living cells, growth factors, and biocompatible chemicals) to build tissue layer by layer. CAD drawings based on MRI or CT images drive this precision machining. Each cell is placed in the desired location, creating a tissue structure that can develop into an organ.
Mimicking the complex structure and function of natural organs is no easy task. Printed tissues require a network of arteries to deliver oxygen and nutrients, so vascularization is essential. Without a vascular network, printed organs will die after transplantation. Fortunately, recent biotechnological solutions emphasize the microvascular system to ensure the vitality and durability of bioprinted objects. Using artificial intelligence, robotics, and biomaterials science, bioprinting can create not only life-supporting structures but also cell clusters.
Biotechnological Breakthroughs Make Bioprinting Possible
In recent years, biotech and academic institutions have made significant advances in organ bioprinting. Organovo, CELLINK, and United Therapeutics are pioneers in 3D bioprinters, bioinks, and tissue engineering. One of the greatest achievements is the printing of small, functional liver tissues that can perform important liver functions and survive in laboratory environments.
Rhythmic heart patches printed from human cells offer hope for cardiac repair therapies. Printing technologies for alveoli, kidney tissue, and pancreatic islets have fueled the development of printing entire organs. The U.S. Food and Drug Administration (FDA) has begun regulatory discussions on bioprinted tissues, indicating a growing interest in applying these technologies to medicine.
As bioprinting becomes more affordable and accessible, personalized organ replacements will use the patient’s own cells. This will significantly reduce the risk of rejection and eliminate lifelong immunosuppression, a major advance in organ transplantation.
Current Medical and Clinical Applications
While organ transplants are still in development, bioprinting is transforming medicine. Skin bioprinting is a popular application. Burn patients and people with chronic wounds benefit from customized skin layers that researchers print. These skin grafts use the patient’s own cells, which speeds healing and reduces complications.
The pharmaceutical industry uses bioprinted tissues for drug screening and toxicology studies. These are more accurate and gentler than animal testing. Scientists can use bioprinted liver tissue to mimic human metabolism and study drug interactions in a controlled laboratory environment. This speeds development and improves preclinical safety.
Bioprinting is also being used in dentistry and orthopedics. Calcium phosphate bone scaffolds, injected with stem cells, are being developed to regenerate jaws, vertebrae, and other skeletal parts. These applications demonstrate how bioprinting can improve function and quality of life in regenerative therapies through customized implants and grafts.
Future Potential and Ethics
The ultimate goal of bioprinting is to create transplantable, fully functional organs. Imagine a world where patients receive personalized organs made from their own cells, and waiting lists for kidneys and hearts are a thing of the past. This groundbreaking technology promises to make this a reality. It is exciting, but it also poses challenges.
Bioprinting must address questions about long-term function, immune response, ethics, and regulation. Will the printed organs grow with the child? Will they adapt to hormonal and environmental changes? Are there socioeconomic implications if bioprinting is limited to affluent areas or private clinics? These scientific questions are accompanied by societal questions.
To ensure ethical implementation, transparent regulations for ownership, distribution, and informed consent are essential, especially for human genetic material. Institutions and governments must work together to defend scientific freedom and human dignity so that bioprinting benefits everyone.
Conclusion
Organ printing based on biotechnology is redefining medicine and life. As we move from experimental models to clinical solutions, technology can eliminate transplant waiting lists, minimize medical inequities, and develop new treatment paradigms. What was once science fiction is evolving into a global medical revolution. With continued research, funding, and ethical scrutiny, organ failure is on the verge of being treated.
We have only scratched the surface of what bioprinting can do. As biotechnology, artificial intelligence, and regenerative medicine converge, lifeprinting will save and change lives. This shift will lead to a healthier, longer, and more equal future for all.
FAQs
1. How does bioprinting work?
Bioprinting uses bioink from living cells to layer biological structures like tissues and organs. With digital models and specialized printers, it can mimic natural anatomy.
2. Will bioprinted organs be used for human transplants?
Fully functional bioprinted organs are not yet used for routine transplants. However, there have been advances in printing skin, cartilage, and liver samples for clinical and pharmacological applications.
3. What are the benefits of bioprinting organs?
Patients can receive customized solutions, reducing organ rejection and eliminating the need for donors. Bioprinting accelerates drug development and research.
4. What are the remaining barriers to mainstream bioprinting?
Vascularization, long-term viability, ethics, cost, and clinical regulatory issues are key issues.
5. When will bioprinting organs be widely available?
Skin and tissue printing is currently in use, but with further development and regulatory approval, full organ transplants could be possible in 10-15 years.